Palliative care is offered by two levels of care providers: primary and specialist. These levels are based on the knowledge and skills of the provider.
View diagram description
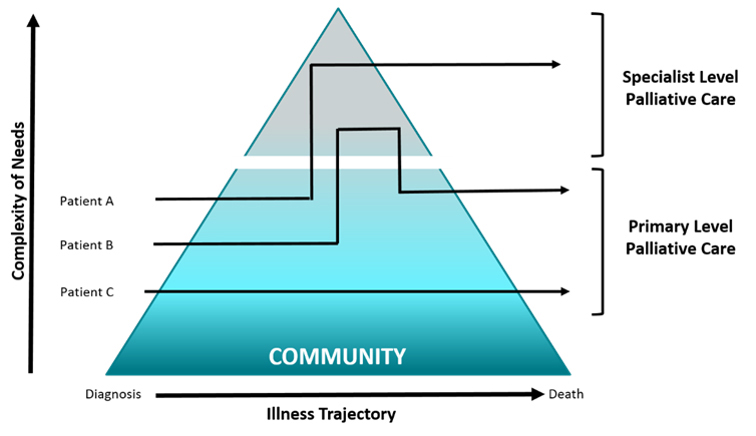
The diagram is a triangle, representing the community of care providers. The base represents the patient’s illness trajectory, from diagnosis to death. The left side represents the patient’s complexity of needs, rising from the bottom to the tip of the triangle. The right side represents the level of care, from none at the bottom, to primary level palliative care in the middle, to specialist level palliative care at the top. Three solid lines show typical trajectories for 3 different patients. See main text for explanation of the trajectories.
The diagram shows how palliative care delivery can change through a person’s illness, as their needs become more complex.
- Complex palliative care needs may require transfer to specialist palliative care teams (Patient A).
- Some palliative care needs may require consultation and clinician-to-clinician support (called “shared care”) by specialist palliative care teams (Patient B).
- Most palliative care needs can be met through primary-level palliative care (known as a “palliative approach to care”) (Patient C). This care may be delivered by many different types of health care providers:
- Primary care clinicians (e.g., family physicians, nurse practitioners, family health teams, nurse practitioner-led clinics, community nurses, home healthcare providers, pain and symptom management consultation teams, emergency care)
- Non-palliative specialist clinicians (e.g., oncologists, internists, geriatricians, pediatricians, respirologists, cardiologists, nephrologists, neurologists, critical care physicians, surgeons)
Adapted from: Advancing High Quality, High Value Palliative Care in Ontario: A Declaration of Partnership and Commitment to Action and Pallium Canada
Model of Care in Ontario
Ideally, an interdisciplinary team of providers work together to deliver palliative care to a patient and their family or caregivers based on their needs.
Each person has unique needs, and because of this, every palliative care team is different. However, each team should include certain members with important roles, such as a most responsible medical provider (physician or nurse practitioner) and a designated care coordinator.
Each team needs to be supported by clinicians who are experts in palliative care and may be physicians, nurses or social workers. The care team might also include other providers such as nurses, disease-specific specialists, social workers, psychologists, spiritual care providers, pharmacists, personal support workers, dietitians, Indigenous providers and volunteers.
To learn more about who should be on a palliative care team, see the Health Services Delivery Framework.
Places Where Palliative Care is Delivered
Palliative care is delivered in a variety of care settings, including the following:
Home
- Provided by home care agencies, visiting hospice care programs or family caregivers.
- Includes nursing care, supporting activities of daily living, social work, case management, and providing medical supplies and equipment as needed.
- Find information about home-based services in your area at healthcareathome.ca/.
Hospital
- Provide more intensive care, and medical treatments to help address complex needs.
- If a person has pain or other symptoms, or they experience a serious change in their health, they may need to visit an emergency department. Some may return home after receiving care, while others may be admitted to the hospital.
- Hospitals may have designated inpatient palliative care units or beds, or they may deliver palliative care in other inpatient units.
- Many hospitals have palliative care consultation teams for patients, as well as other patient and caregiver programs and supports.
Hospice
- A community-based organization (or program) that supports people living with a progressive, life-limiting illness and their caregivers, family members and friends.
- Provides support in a variety of settings, including a person’s home or a homelike setting.
- Offers services such as hospice-trained volunteers, day programs, psychosocial supports, grief and bereavement support, spiritual care, caregiver support, wellness programs, complementary therapies, children’s programs, outreach or shared-care teams, and end-of-life care within a hospice residence.
Hospice Residence
- A health care facility and registered charity that offers palliative care services by an inter-professional team with palliative care expertise.
- Care is available 24 hours a day, 7 days a week in a home-like setting for the individual and their significant others.
Long-Term Care Home
- Places where adults can live and get help with most of their daily activities (e.g., eating, bathing)
- Provides access to 24-hour nursing care including palliative care.
- Best suited for people with significant health challenges.
- Offers palliative care to residents unless they need to be admitted to hospital due to medical complications.
- To learn more about long-term care homes and eligibility criteria, visit the long-term care overview on the Ontario website.
Palliative care may also be provided in other places where people live together, such as retirement homes.
Find Palliative Care Support and Services in Your Area
If you are a patient, caregiver or family member looking for local palliative care support, connect with your primary care provider.
For information about palliative care resources and programs in your area, visit the “Home Health and Community Supports” page and “End-of-Life Care” page at thehealthline.ca/.